Background
As new technologies emerge and patient expectations change, pharmacists and pharmacy technicians (regulated members) have seen a shift in how prescriptions are transmitted from prescriber to regulated member. Although there are different methods that are acceptable, regardless of the method used, regulated members are required by Standard 6 of the Standards of Practice for Pharmacists and Pharmacy Technicians to always ensure that the prescription is current, authentic, complete, and appropriate before dispensing. Additionally, regulated members have a responsibility to protect the confidentiality of the patient and to ensure that accurate records are created and maintained in the dispensary of the pharmacy or an approved off-site storage.
Advice to protect you, your patients, and your profession
When accepting prescriptions, pharmacists and pharmacy technicians should consider the following:
- Acceptable methods of prescription transmission
- Prescriptions can be provided to pharmacies in various formats:
- handwritten, signed, and provided directly to the patient to be presented at the pharmacy or faxed directly to the pharmacy from the prescriber;
- produced by computer and hand-signed by the prescriber or affixed with an electronic signature that is hand-initialled by the prescriber, and then provided directly to the patient to be presented at the pharmacy or faxed directly to the pharmacy from the prescriber;
- faxed directly from the prescriber via a password-protected electronic medical record (EMR) or system such as Connect Care;
- issued and transmitted from the prescriber via secure messaging in a closed electronic system (e.g., PrescribeIT) that enables monitoring and shared access by authorized prescribers and dispensers1; or
- provided verbally by telephone to an authorized regulated member by the prescriber or their authorized intermediary2.
- Prescriptions can be provided to pharmacies in various formats:
- Signatures
- Purpose of signature. A valid signature assists the regulated member in verifying the authenticity of a written prescription.
- Signatures – hand-written and electronic.
- An acceptable hand-written signature is one that is unique to each prescription and signed by the prescriber at the time the prescription is written. This signature can be:
- signed or initialed by the prescriber using a pen, or
- a digitally captured hand-signed signature that is unique to each prescription and captured by an electronic device at the time of prescribing.
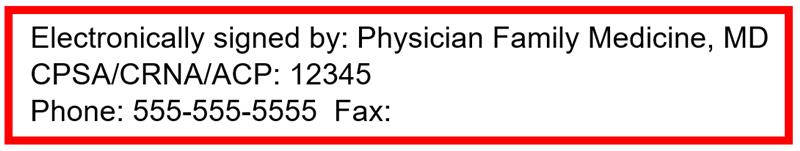
- An acceptable electronic signature is a unique digital signature generated by a password-protected system such as Connect Care or a password-protected EMR, using the prescriber’s credentials that function as the method of direct authorization. E.g. the example below:
- Note: A computer generated electronic reproduction of a hand-written signature is not acceptable unless it is signed or initialled (digitally or in ink) by the prescriber at the time it is written.
- When a hand-written signature is needed. A hand-written signature or initial is required when
- prescriptions are provided directly to the patient by the prescriber, or
- prescriptions are generated in a system that is not closed and secure.
- When a hand-written signature is not required. If a regulated member is uncertain about the authenticity of a prescription, they should take steps such as calling or faxing the prescriber to be certain that the prescriber’s EMR meets the requirements before accepting the prescription. A hand-written signature is not required when
- prescriptions are faxed directly to a pharmacy from a password-protected system such as Connect Care or a password-protected EMR, since the prescriber’s credentials function as the method of direct authorization, or
- prescriptions are directly transmitted to the pharmacy using secure messaging in a closed electronic system such as PrescribeIT.
- An acceptable hand-written signature is one that is unique to each prescription and signed by the prescriber at the time the prescription is written. This signature can be:
- Tracked Prescription Program (TPP) drugs. The rules of TPP Alberta require that type 1 TPP drugs can only be accepted if provided on a signed TPP form that is provided to the patient or faxed to the pharmacy, unless the prescriber is practicing at a facility or within a program that has been granted an exemption by TPP. If the facility or program has been granted an exemption by TPP, the advice in this document applies.
- Patients providing an image or description of a prescription to a regulated member in advance.
- The original prescription must be received by the pharmacy via one of the acceptable methods of transmission. Regulated members cannot meet the standards for conducting an assessment, creating a patient record, entering information into Netcare, or dispensing the medication when they do not have the original prescription. Being provided an image by text message, email, or mobile app, or the patient reading a prescription over the phone or faxing a copy to the pharmacy is not acceptable.
- Establish a professional relationship. It is not appropriate for a pharmacist to complete an assessment and dispense a prescription without establishing a professional relationship with the patient or their designate that enables the pharmacist to confirm their identity when receiving the filled prescription.
- Avoid errors. Processing and preparing a prescription before obtaining the original increases the risk of error and diversion. As it is the patient who is responsible for taking the photograph of the original prescription, there is the potential that relevant material on the prescription may be inadvertently removed leading to error, or purposefully removed leading to diversion.
- Avoid creation of duplicate records. Processing and preparing a prescription before obtaining the original may lead to the creation of false, inaccurate, or duplicate records. With more and more pharmacies relying on real-time integration with Netcare, this problem is accelerated because processing a prescription means a record is created immediately in Netcare. Regulated members must receive and retain the original prescriptions before any records are created or uploaded to Netcare. The following are examples of how records may become inaccurate:
- If the pharmacy processes a prescription without the original and the patient then takes the original to another pharmacy, duplicate records may be created with both the patient’s Netcare records and third-party insurer records.
- A time delay between the time of processing and pickup may lead to a record created in Netcare without the pharmacist having confirmed the authenticity of the prescription.
Further reading
- Per federal regulations, pharmacy technicians may not accept verbal prescriptions for controlled substances. ↩︎
- There is greater risk associated with the use of intermediaries and this method of prescription transmission should only be used if other methods are unavailable and a delay in transmission might harm patient care. ↩︎

